Some insurance companies haven’t been shy about their criticisms of Obamacare lately, giving conservatives fodder for their political arguments that the law is a failure that is destroying the entire health care market.
But there is more going on than the surface level threats to leave ACA exchanges amid accusations that they’re not sustainable. These complaints are not just reflections of issues that insurers have had in adapting to the new law, but a way to influence how it evolves in the future, health care experts told TPM.
In other words, health insurance companies are settling in for the long haul and using a combination of public and private advocacy that is very familiar to other industries regulated at the federal level.
Adding to the current dynamic is the upcoming election. A new Congress and president, especially a Republican in the White House, could have major implications for the law and for the requirements the Department of Health and Human Services places on insurers.
“You can bet those insurers will make sure that they’re at the table and have as much leverage as possible,” Larry Levitt, vice president at the Kaiser Family Foundation, said in an interview with TPM. “Creating an environment where people are worried about insurers losing money and whether they’ll participate in the marketplaces or not increases their leverage.”
UnitedHealth made headlines in November, when officials said on a call with investors that it was considering leaving the ACA exchanges entirely because of the losses incurred there.
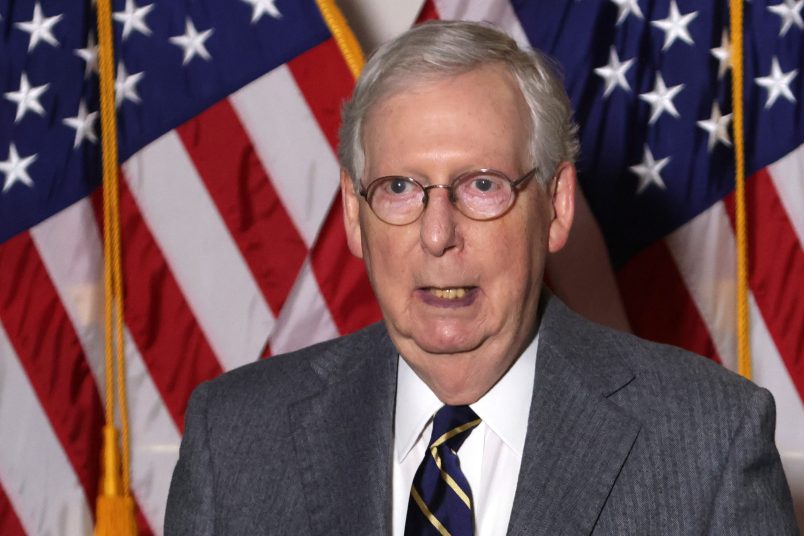
“We cannot sustain these losses,” UnitedHealth CEO Stephen Hemsley (pictured above on the right) said then. The insurance company has yet to confirm its final plans, but its losses have fed into accusations that the marketplaces aren’t working.
The gloom-and-doom refrains returned when Aetna said this week it had “serious concerns” about exchanges. Chief Executive Officer Mark Bertolini (pictured above on the left) told investors that the government “has made some recent changes but more needs to be done.”
It’s true that some insurers fared worse than others adapting to the marketplaces, but growing pains were expected with the ACA, and some insurers are reasonably optimistic about their prospects on the exchanges.
The losses that UnitedHealth incurred in particular are indeed very real, but also to some extent self-inflicted, according to experts.
“UnitedHealth’s complaints are real,” Caroline Pearson, senior vice president at Avalere Health, told TPM. “But that doesn’t mean that the whole market is collapsing.”
For many reasons, UnitedHealth’s circumstances were different than other insurers: it sat out of the exchange for a year, the individual market was never a significant interest of their company, and their plans were mis-priced for the competition, experts said.
Peter Lee, the director of California’s exchange, accused UnitedHealth of using the ACA as scapegoat for its own miscalculations.
“Instead of saying, ‘We screwed up,’ they said, ‘Obamacare is the problem and we may not play anymore,’ ” Lee said in an interview with California Healthline. “It was giving an excuse to Wall Street and throwing the Affordable Care Act under the bus.”
Other insurers have had issues, but their complaints are also geared to obstacles they foresee in the future.
“They’re going to highlight the challenges they’ve had in the market because they’ve got increased regulatory pressure coming down the pike,” Pearson said, pointing to government’s Notice of Benefit and Payment Parameters for 2017, which outlines its proposed future regulations.
“[The proposal has] lots of additional regulatory requirements that the health plans do not like,” Pearson said. “But they’ve also said, ‘We’re not fleeing this market.’”
A source that works with the insurance industry called the proposed regulations “a dramatic departure from where we are” and pointed to them when asked about the complaints some insurers are making.
“There’s the fact that there’s still the regulatory landscape that continues to evolve. We’re still having to deal with new regulations coming out,” she said.
A major point of contention between industry and regulators is special enrollment periods, which let certain people enroll in plans outside of the typical open enrollment period.
“The insurers have been consistently pointing to the special enrollment periods recently,” Levitt said. “I think that’s no accident. That’s a live policy issue. Blaming losses on special enrollment is a way to potentially influence policy and also to deflect blame from any missteps they may have made.”
Insurers are also pushing back against standards imposed on the benefits they offer, as well as how they deal with out-of-network care.
“In general, insurers are looking to exercise more control over how insurers market [coverage] and how consumers buy it,” Levitt said.
But companies’ griping should not be taken as a sign that the industry is preparing to jump ship on the ACA — a law insurance companies helped create that has brought them millions of new consumers.
“They want to be at the table. They want to be engaged. They want to make it work. They want to participate in the markets,” Pearson said. “It’s also really important that they make it clear that it hasn’t been easy, that any dramatic increase in regulation from the government is going to make the market less attractive to them.”